University of Pittsburgh Neuroscience Research Highlights
Pitt began making strides in neuroscience research more than 60 years ago when Jonas Salk and his team sought to end the threat of polio virus, which attacks the brain and spinal cord to cause in the most severe cases muscle weakness, paralysis and death. In April 1955, Salk and his colleagues announced that the vaccine they developed prevented polio in most of those who received it in a nationwide trial, heralding the end of epidemics that until then had killed or crippled 35,000 people annually. The vaccine, made of inactivated virus, primed the immune system to recognize and eliminate the live germ before harm could be done. The Salk vaccine was administered to millions of children in subsequent years, contributing to the eradication of polio in the Western hemisphere by 1994.
Over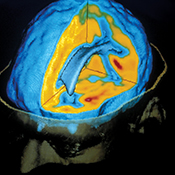 the course of the past decade, the University of Pittsburgh School of Medicine’s Chester Mathis, Pitt Distinguished Professor of Radiology, and William Klunk, Distinguished Professor of Psychiatry and Neurology, developed and refined Pittsburgh Compound B (PiB). This radioactive tracer, used in concert with positron emission tomography (PET) scanning, can detect the formation of amyloid plaque—a hallmark of Alzheimer’s disease—in the living brain. Before their breakthrough, the only way to confirm the presence of this plaque was through autopsy. PiB has been licensed to GE Healthcare, which recently received approval to market in the U.S. a PiB analog to image amyloid plaque in patients. Approval for its use in Europe and Asia is currently under regulatory review.
the course of the past decade, the University of Pittsburgh School of Medicine’s Chester Mathis, Pitt Distinguished Professor of Radiology, and William Klunk, Distinguished Professor of Psychiatry and Neurology, developed and refined Pittsburgh Compound B (PiB). This radioactive tracer, used in concert with positron emission tomography (PET) scanning, can detect the formation of amyloid plaque—a hallmark of Alzheimer’s disease—in the living brain. Before their breakthrough, the only way to confirm the presence of this plaque was through autopsy. PiB has been licensed to GE Healthcare, which recently received approval to market in the U.S. a PiB analog to image amyloid plaque in patients. Approval for its use in Europe and Asia is currently under regulatory review.
In 1986, Andrew Schwartz, a professor of neurobiology in the School of Medicine, had an idea he was sure would work: translating signals in the brain, so a person’s thought could move a very high-tech prosthetic limb. In December 2012, it worked very well as a result of a collaborative effort including Schwartz, Michael Boninger, (Physical Medicine and Rehabilitation), Elizabeth Tyler-Kabara (Neurological Surgery), and Jennifer Collinger (Physical Medicine and Rehabilitation). After months of training, Jan Scheuermann, a 53-year-old mother of two whose ability to move below the neck was stolen by a neurodegenerative condition, fed herself a chocolate bar with a robotic arm. The brain-control interface uses a microelectrode array—in this case, a 16-square-millimeter grid with 96 points penetrating the brain by one-sixteenth of an inch—to connect brain cells to electronic circuitry, which translate thought to action. Schwartz and his colleagues are trying to further refine the arm by using brain-computer interface technology to generate sensation in the brain, allowing the arm’s user to adjust grip strength.
The human brain has 40 major fiber tracts, neural pathways that connect distant regions to one another, permitting all manner of complex forms of cognition. These fibers can be clearly observed post-mortem, which is of little help to surgeons looking for the least harmful way to excise a tumor or for doctors hoping to precisely quantify the damage wrought by traumatic brain injury and predict the potential for successful rehabilitation. A newly developed imaging technique called high-definition fiber tracking (HDFT)—which uses advanced computational means to process data from high-tech MRI machines—permits doctors to pinpoint pathways in a living patient. In addition to other applications of HDFT, Walter Schneider, Pitt professor of psychology and neurosurgery and senior scientist at Pitt’s Learning Research and Development Center; Juan Fernandez-Miranda, assistant professor of neurological surgery at Pitt and director of the University’s Surgical Neuroanatomy Lab; and David Okonkwo, associate professor neurological surgery and director of the Neurotrauma Program, in collaboration with Pitt’s neurosurgeons, refined HDFT so as to allow a safer and more effective surgical approach to brain lesions that have been difficult to access without damaging vital fiber tracts.
Other Stories From This Issue
On the Freedom Road

Follow a group of Pitt students on the Returning to the Roots of Civil Rights bus tour, a nine-day, 2,300-mile journey crisscrossing five states.
Day 1: The Awakening
Day 2: Deep Impressions
Day 3: Music, Montgomery, and More
Day 4: Looking Back, Looking Forward
Day 5: Learning to Remember
Day 6: The Mountaintop
Day 7: Slavery and Beyond
Day 8: Lessons to Bring Home
Day 9: Final Lessons

